ECHO-203: IDO1 and PD-L1 inhibition in advanced solid tumors
An immunotherapy treatment combining the IDO1 inhibitor epacadostat and the PD-L1 inhibitor durvalumab was found to be safe in patients with advanced solid tumors, with safety data similar to treatment with durvalumab alone, according to data presented from the ongoing ECHO-203 clinical trial at the AACR Annual Meeting 2018.
Aung Naing, MD, FACP, associate professor, Department of Investigational Cancer Therapeutics, Division of Cancer Medicine, The University of Texas MD Anderson Cancer Center, Houston and colleagues tested the combinatorial treatment in 34 patients with advanced pancreatic cancer, melanoma, non-small cell lung cancer (NSCLC), or squamous cell carcinoma of the head and neck (SCCHN). Exclusion criteria included prior checkpoint inhibition therapy for any unapproved indications.
Patients received doses of epacadostat ranging from 25 to 300mg twice daily in combination with 3 or 10mg/kg of durvalumab every two weeks. Safety data were compiled from patients who received at least one treatment dose. One dose-limiting toxicity (DLT) was observed.
Common adverse events (AEs) included fatigue (32 percent), pruritus (severe itching; 15 percent), diarrhea, nausea, and rash (12 percent each); five patients discontinued treatment due to AEs.
“This is the first report of IDO1 inhibition in combination with PD-L1 antagonism, and we found that epacadostat plus durvalumab was generally well-tolerated in patients with advanced cancers, with a safety profile consistent with previous reports of durvalumab monotherapy,” said Naing. “Prior preclinical work suggested that dual inhibition of both IDO1 and the PD-1/PD-L1 axis was more efficacious than targeting either component alone”, noted Naing. “These studies laid the foundation for the human trials of agents that target the PD-1/PD-L1 pathway and IDO1,” he explained.
As of Oct. 29, 2017, efficacy data for 15 patients with advanced pancreatic cancer treated at various dose levels revealed no responses. Four patients had stable disease, resulting in a disease control rate of 27 percent; one patient discontinued treatment following clinical progression.
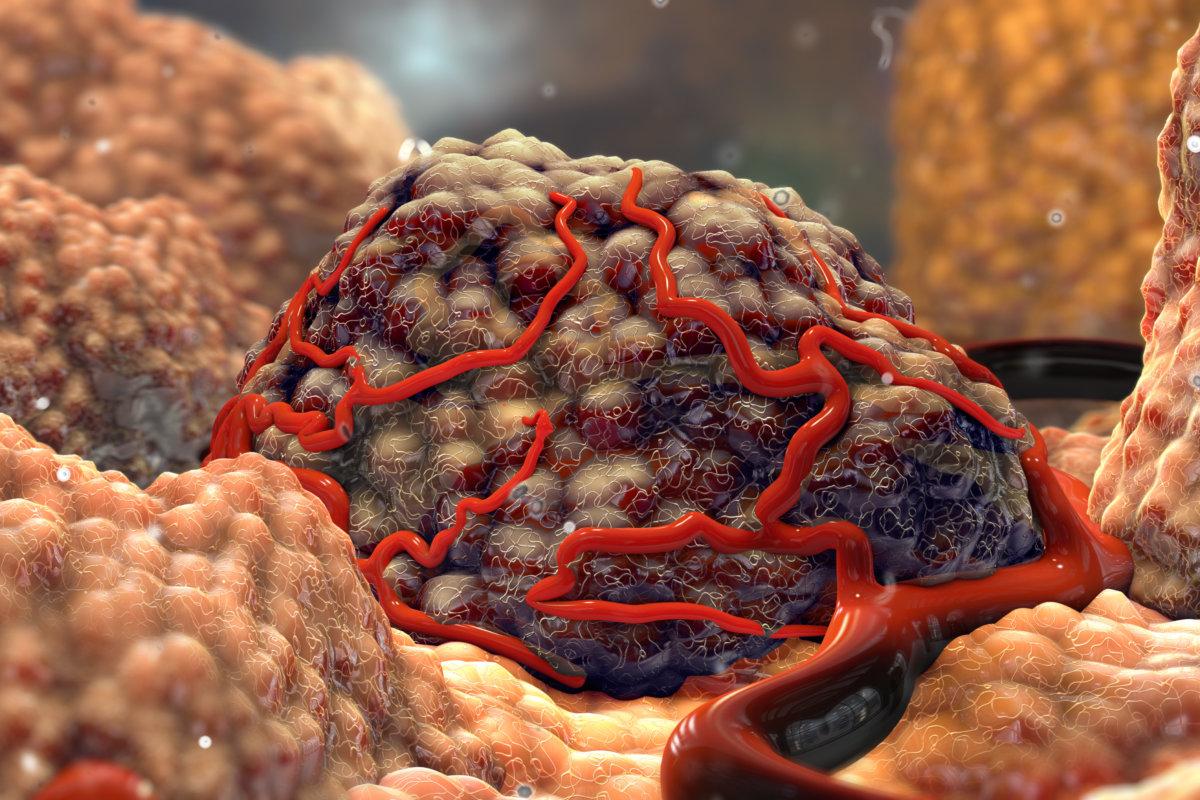
“Because pancreatic cancer has an immunosuppressive tumor microenvironment that generally excludes T cells, combinatorial therapies that enhance the immune response will be needed for an effective immunotherapeutic regimen,” explained Naing.
“However, as pancreatic cancer is not generally responsive to immunotherapy, these results were not a complete surprise,” he noted. “We found that epacadostat drug levels were slightly lower in pancreatic cancer patients who had prior pancreatic and duodenal surgeries, which are commonly performed in this patient population.”
Phase II expansions, with epacadostat doses of 100 and 300mg in combination with 10mg/kg of durvalumab, are currently being evaluated in patients with NSCLC, SCCHN, and urothelial carcinoma. “Since these tumor types have demonstrated efficacy with checkpoint inhibition monotherapy, they were considered more likely to potentially benefit from combination immunotherapy,” noted Naing.